The Importance of Timing in Fertility Evaluation: When Should Couples Start Investigating Infertility?
Fertility is a complex biological process influenced by hormonal, genetic, anatomical, and lifestyle factors. One of the most critical—but often misunderstood—elements in fertility care is timing. Knowing when to start a fertility evaluation has a direct impact on diagnosis, treatment success, and long-term reproductive outcomes.
Global organizations such as the World Health Organization (WHO), the American Society for Reproductive Medicine (ASRM), and the European Society of Human Reproduction and Embryology (ESHRE) emphasize that age plays a central role in determining the appropriate timing for infertility evaluation.
This article explains, in detail, the scientific recommendations regarding when couples should begin fertility investigations, why age matters, and which high-risk groups require immediate assessment.
WHO Definition of Infertility
According to the World Health Organization:
Infertility is defined as the failure to achieve pregnancy after 12 months of regular, unprotected intercourse.
(WHO Infertility Definition, 2020 Update)
While this definition provides a general framework, WHO offers more specific guidance depending on age and medical history.
1. Couples Under Age 35
For couples where the female partner is younger than 35 years, fertility potential is still considered within the normal range.
WHO Recommendations:
- 0–6 months of trying: No testing needed; considered normal.
- 6–12 months: Early evaluation is optional.
- After 12 months: A complete fertility evaluation is recommended.
Why wait up to 12 months?
Because:
- Egg quality is typically optimal under age 35.
- Ovarian reserve is generally adequate.
- Sperm parameters tend to be within normal ranges.
- Many couples conceive naturally within the first year.
However, failure to conceive after 12 months strongly suggests an underlying issue, making further delay inappropriate.
2. Women Over Age 35: Evaluation After 6 Months
Global fertility guidelines uniformly state:
If a woman is 35 or older, fertility evaluation should begin after 6 months of trying without success.
The biological explanation:
After age 35:
- Egg quality declines more rapidly.
- Ovarian reserve markers (AMH and AFC) decrease significantly.
- Chromosomal abnormalities in eggs become more common.
- Time-sensitive fertility declines accelerate.
Waiting a full year—appropriate for younger women—can be detrimental in this age group. Early assessment provides a crucial opportunity for timely intervention and may prevent the need for more complex treatments later.
3. High-Risk Groups Who Should Not Wait
WHO and ASRM emphasize that certain individuals should seek immediate fertility evaluation, regardless of age or duration of trying.
These include:
- Women with very irregular cycles or amenorrhea
- History of ovarian surgery
- Very low AMH or low AFC detected previously
- Moderate to severe endometriosis
- A history of pelvic inflammatory disease
- Prior chemotherapy or radiation
- Known male factor infertility
- Thyroid disorders that are uncontrolled
- History of recurrent miscarriages
For these individuals, waiting—even for 6 months—may result in significant loss of reproductive potential.
4. Why Early Diagnosis Is Essential
Scientific research consistently shows that early fertility evaluation leads to:
- A higher probability of successful treatment
- Lower financial and emotional burden
- Prevention of unnecessary medical interventions
- More personalized treatment plans
In contrast, delayed diagnosis often leads to:
- Reduced ovarian reserve
- Higher need for IVF or advanced reproductive technologies
- Increased emotional stress
- Lower success rates
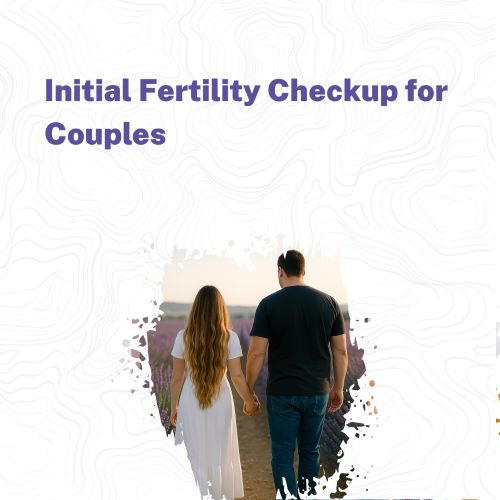
5. What Does an Initial Fertility Evaluation Include?
A proper diagnostic workup involves evaluating both partners.
A. Female Evaluation
Includes:
- Hormonal testing: AMH, FSH, LH, Estradiol, TSH, Prolactin
- Transvaginal ultrasound: Assessment of ovarian reserve via AFC
- Ovulation assessment: Regularity of menstrual cycles
- Uterine and tubal evaluation: Sonography, HSG if required
These tests help identify ovulatory disorders, diminished ovarian reserve, uterine abnormalities, or tubal blockages.
B. Male Evaluation
The first and most important test is a WHO-standard semen analysis, measuring:
- Volume
- Concentration
- Total sperm count
- Motility
- Morphology
- Vitality
Because 50% of infertility cases involve male factors, ignoring male testing delays diagnosis and treatment.
6. Common Misconception: Starting Treatment Without Diagnosis
One of the most frequent clinical mistakes is beginning treatment—such as ovulation induction, IUI, or even IVF—without first conducting a thorough evaluation.
Evidence shows:
- Nearly 30% of infertility causes are simple hormonal problems that can be corrected.
- 50% involve male factors, which may not require IVF if properly diagnosed.
- 20% are combined factors, requiring tailored treatment.
Accurate diagnosis is the cornerstone of effective fertility care.
7. The Role of Age in Long-Term Fertility Planning
Age affects not only natural conception but also:
- Response to fertility medications
- IVF success rates
- Embryo quality
- Risk of miscarriage
- Risk of chromosomal abnormalities
Therefore, knowing when to initiate evaluation helps preserve reproductive potential and improve outcomes.
Conclusion
Timing is one of the most crucial elements in fertility assessment.
According to WHO:
- Under 35: Evaluate after 6–12 months
- Over 35: Evaluate after 6 months
- High-risk groups: Evaluate immediately
Early diagnosis means:
- A shorter treatment path
- Higher success rates
- Lower emotional and financial stress
- More efficient reproductive planning
Understanding these guidelines empowers couples to take informed, proactive steps toward achieving a healthy pregnancy.