Can conception fail?
Conception is the biological process in which a sperm fertilizes an egg to create the first cell of a new human life. While this process may sound simple, it is in fact highly complex and depends on precise timing, healthy reproductive cells, and properly functioning reproductive organs. For many individuals and couples, conception does not occur immediately—or at all—despite regular unprotected intercourse. This can be confusing and emotionally challenging, but it is also very common.
Conception failure does not necessarily indicate permanent infertility. In many cases, it is the result of identifiable and sometimes treatable factors. Understanding why conception can fail is the first step toward addressing fertility challenges and choosing appropriate next steps.
1. Poor Timing or Infrequent Intercourse
One of the most common and underestimated reasons for conception failure is poor timing. Conception can only occur when both the egg and sperm are present and viable at the same time.
- After ovulation, a released egg survives for only 12 to 24 hours.
- Sperm cells, on the other hand, can survive inside the female reproductive tract for up to five days under optimal conditions.
Because of this difference, the fertile window usually includes the five days before ovulation and the day of ovulation itself. Intercourse that occurs too early or too late outside this window significantly reduces the chances of fertilization.
Additionally, infrequent intercourse can lower the probability of conception. While daily intercourse is not required, having sex only occasionally—especially without awareness of ovulation timing—can make conception unlikely even when both partners are fertile.
2. Low Sperm Quality or Quantity
Healthy sperm are essential for successful conception. Even when timing is perfect, conception may fail if sperm quality or quantity is compromised. Several key sperm parameters influence fertility:
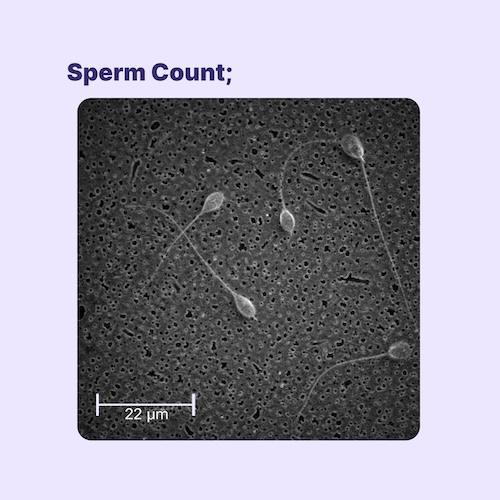
- Sperm count: Too few sperm reduce the likelihood that one will reach and fertilize the egg.
- Motility: Sperm must be able to swim effectively through the female reproductive tract.
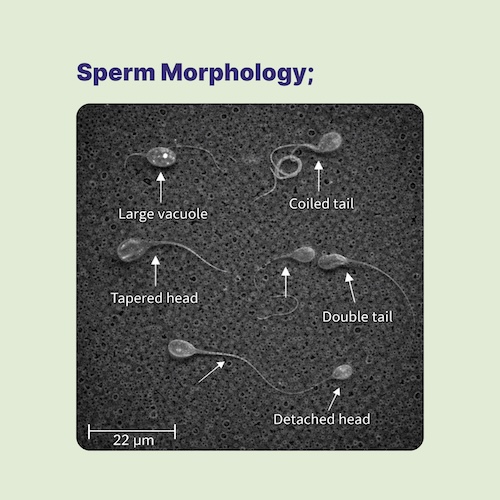
- Morphology: Abnormal shape or structure of the sperm head or tail can impair fertilization.
- DNA integrity: Damage to sperm DNA can prevent fertilization or lead to early pregnancy loss.
Low sperm quality may result from infections, hormonal imbalances, medications, smoking, alcohol use, obesity, chronic stress, exposure to toxins, advanced age, or genetic conditions.
3. Poor Egg Quality or Low Egg Reserve
Just as sperm health matters, egg quality plays a crucial role in conception. A healthy egg must contain the correct number of chromosomes and have a normal internal structure to support fertilization and early development.
Egg quality naturally declines with age, especially after the mid-30s. Over time, eggs are more likely to have chromosomal abnormalities, which can prevent fertilization, implantation, or result in early miscarriage. Other factors that may affect egg quality include hormonal disorders, autoimmune conditions, metabolic diseases, and lifestyle factors such as poor nutrition or prolonged stress.
In some individuals, the quantity of available eggs (ovarian reserve) is also reduced, making ovulation less frequent or unpredictable.
4. Blocked or Damaged Fallopian Tubes
In natural conception, fertilization typically occurs in the fallopian tubes, which connect the ovaries to the uterus. These tubes must be open and functional for sperm to reach the egg and for the fertilized egg to travel to the uterus.
Fallopian tubes can become blocked or damaged due to:
- Pelvic inflammatory disease (PID)
- Sexually transmitted infections
- Endometriosis
- Previous abdominal or pelvic surgeries
When the tubes are blocked, sperm cannot reach the egg, or a fertilized egg cannot reach the uterus. This makes natural conception impossible without medical intervention.
5. Hormonal Imbalances and Ovulation Problems
Hormones regulate ovulation, sperm production, and preparation of the uterus for pregnancy. If hormone levels are disrupted, conception may fail even if reproductive organs appear normal.
Conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, or elevated prolactin levels can interfere with ovulation. Without regular ovulation, the egg may not be released at all, eliminating the chance of conception during that cycle.
6. Genetic and Chromosomal Factors
Even when fertilization occurs, conception may not lead to a viable pregnancy if there are genetic or chromosomal abnormalities. Errors in chromosome number or structure can prevent implantation or cause very early pregnancy loss. These events are common and often occur without noticeable symptoms.
7. Environmental and Lifestyle Factors
Environmental exposures and lifestyle choices can significantly affect fertility. Smoking, excessive alcohol consumption, poor sleep, chronic stress, obesity, and exposure to environmental toxins may impair sperm function, egg quality, or hormonal balance.
When to Seek Medical Advice
If conception has not occurred after 12 months of regular unprotected intercourse (or after 6 months for individuals over 35), consulting a healthcare provider is recommended. Fertility evaluations can help identify underlying causes of conception failure and guide appropriate treatment options, which may include lifestyle changes, medications, or assisted reproductive technologies.
Conception Failure Is Not the End
Conception is a delicate process influenced by many biological, hormonal, and environmental factors. Failure to conceive does not mean failure as a person or couple. With proper evaluation, medical support, and accurate information, many causes of conception failure can be addressed, and alternative paths to pregnancy can be explored.