Why Does Sperm Shape Matter in Fertility?
Introduction
When discussing male fertility, most people immediately focus on sperm count. Others may be familiar with sperm motility. However, fertility is not determined by numbers alone. Even when sperm count and motility fall within normal ranges, fertilization may still fail. One critical yet often misunderstood factor is sperm morphology — the shape and structural integrity of sperm cells.
According to the World Health Organization (WHO), sperm morphology is one of the three core parameters evaluated in semen analysis, alongside sperm concentration and motility. Clinical guidelines from the American Society for Reproductive Medicine (ASRM) and the European Association of Urology (EAU) emphasize that abnormal sperm morphology can influence fertilization rates, embryo development, and pregnancy outcomes.
Understanding sperm morphology helps provide a more complete picture of male reproductive health.
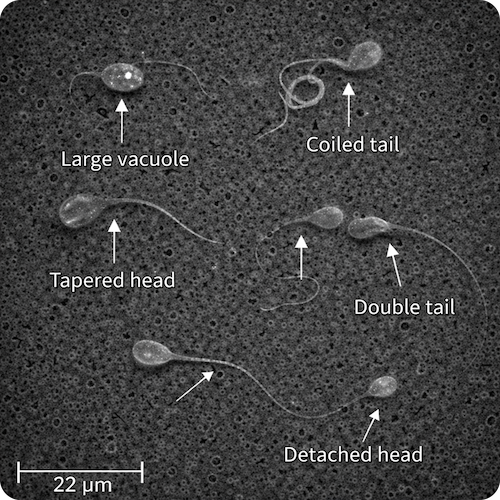
What Is Sperm Morphology?
Sperm morphology refers to the size, shape, and structural characteristics of sperm cells when examined under a microscope. During laboratory evaluation, semen samples are stained and analyzed to determine the percentage of sperm that meet strict criteria for normal structure.
According to the latest WHO laboratory manual (6th edition), the lower reference limit for normal morphology is 4% using strict criteria (Kruger criteria). This means that even in fertile men, a large proportion of sperm may appear abnormal. However, having at least 4% normally shaped sperm is statistically associated with a reasonable probability of natural conception.
It is important to note that morphology assesses structural appearance — not directly genetic quality — although structural abnormalities may sometimes correlate with DNA damage.
The Structure of a Normal Sperm Cell
A healthy sperm cell consists of three essential parts:
1. The Head
The sperm head should be:
- Smooth and oval in shape
- Symmetrical
- Properly proportioned
- Equipped with an intact acrosome
The head contains the paternal DNA. The acrosome, a cap-like structure at the tip of the head, holds enzymes necessary to penetrate the egg’s outer protective layer (zona pellucida). Abnormalities in head shape may impair egg penetration or proper genetic delivery.
2. The Midpiece
The midpiece:
- Connects the head and tail
- Contains mitochondria
- Supplies energy for movement
Structural defects in the midpiece may reduce energy production, leading to impaired motility and reduced fertilization potential.
3. The Tail
The tail:
- Should be long, straight, and uncoiled
- Enables forward movement
- Propels the sperm toward the egg
Any defect in the tail may significantly impair the sperm’s ability to swim effectively through the female reproductive tract.
Common Morphological Abnormalities
Abnormal morphology may affect one or more sperm components.
Head Abnormalities
- Round head (Globozoospermia)
- Double head
- Large or small head
- Absent or defective acrosome
- Large vacuoles
These abnormalities may interfere with egg penetration, fertilization, or early embryo development.
Midpiece Abnormalities
- Thickened midpiece
- Bent midpiece
- Irregular mitochondrial arrangement
These defects often compromise energy supply and reduce motility efficiency.
Tail Abnormalities
- Short tail
- Coiled tail
- Double tail
- Broken tail
Such abnormalities directly impair motility and the sperm’s ability to reach the egg.
Why Does Sperm Morphology Matter for Fertilization?
Fertilization is a complex, multi-step biological process. For successful conception, sperm must:
- Travel through the cervix
- Navigate the uterus
- Reach the fallopian tube
- Bind to the zona pellucida
- Penetrate the egg
- Deliver intact genetic material
Abnormal morphology may compromise one or more of these steps.
Several studies suggest that severe teratozoospermia (very low normal morphology) may be associated with:
- Reduced fertilization rates
- Lower blastocyst formation
- Increased early pregnancy loss
- Reduced IVF success rates
However, the relationship is complex. Some men with low morphology still achieve natural pregnancies, highlighting the importance of evaluating all semen parameters together.
Does Morphology Alone Determine Fertility?
No.
No major clinical guideline recommends diagnosing infertility based solely on sperm morphology. Fertility evaluation must include:
- Sperm count
- Sperm motility
- Semen volume
- Hormonal profile
- Medical history
- In some cases, sperm DNA fragmentation testing
Morphology is one piece of a larger diagnostic puzzle.
Can Sperm Morphology Be Improved?
In many cases, yes.
Spermatogenesis (sperm production) takes approximately 70–90 days. Therefore, lifestyle changes may show measurable improvements within three months.
Evidence-based strategies that may support improved morphology include:
- Smoking cessation
- Reducing alcohol intake
- Weight management
- Regular moderate exercise
- Antioxidant supplementation (e.g., zinc, selenium, CoQ10, vitamin D)
- Stress reduction
- Treating underlying conditions such as varicocele
Environmental exposure reduction (e.g., avoiding excessive heat, minimizing plastic BPA exposure) may also be beneficial.
Clinical Perspective
It is crucial to interpret morphology results within context. A slightly reduced morphology percentage does not automatically mean infertility. Similarly, a normal morphology result does not guarantee fertility.
Modern reproductive medicine emphasizes a comprehensive, individualized assessment rather than reliance on a single parameter.
Conclusion
Sperm morphology is a vital indicator of male reproductive health. While it does not determine fertility on its own, it plays a significant role alongside sperm count and motility.
Understanding sperm shape helps couples make informed decisions, seek timely medical advice, and approach fertility evaluation with scientific clarity rather than anxiety.
Male fertility is multidimensional — and morphology is a critical part of that equation.