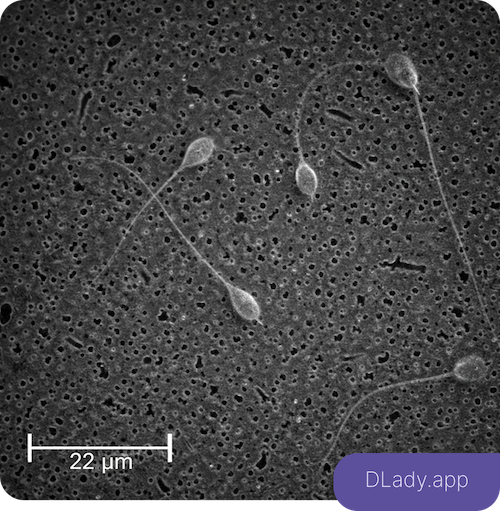
What Is Sperm Count and Why Does It Matter for Male Fertility?
In previous articles, we discussed sperm morphology (shape) and its role in male fertility in detail.
However, evaluating male reproductive health is not limited to sperm shape alone. Another fundamental and widely reported parameter in semen analysis is sperm count—often the first number that draws attention on a lab report.
In this article, we focus specifically on sperm count: what it means, how it is measured, its normal reference ranges, and why it must always be interpreted alongside other parameters and based on reliable international guidelines.
Scientific Definition of Sperm Count in Semen Analysis
According to laboratory standards published by the World Health Organization (WHO), sperm count is usually reported in two ways:
1. Sperm Concentration
The number of sperm present in each milliliter of semen, typically expressed as million sperm per milliliter.
2. Total Sperm Count
The total number of sperm in the entire ejaculate, calculated by multiplying sperm concentration by semen volume.
In clinical practice, sperm concentration is often the primary parameter used for interpretation, as it allows for more accurate comparison across individuals.
Normal Sperm Count Ranges Based on International Guidelines
According to the latest WHO laboratory manual for semen analysis, the lower reference limits are:
- Normal sperm concentration: ≥ 15 million/mL
- Normal total sperm count: ≥ 39 million per ejaculate
Values below these thresholds are categorized as:
- Oligospermia: reduced sperm count
- Severe oligospermia: markedly reduced sperm count
- Azoospermia: complete absence of sperm in semen
It is important to note that these values are reference limits, not absolute cutoffs. They are based on population data from fertile men and must be interpreted cautiously.
Does a High Sperm Count Guarantee Fertility?
One of the most common misconceptions is that a normal or high sperm count automatically means fertility is guaranteed.
However, clinical guidelines from the American Society for Reproductive Medicine (ASRM) and the American Urological Association (AUA) clearly emphasize that:
Sperm count alone is not sufficient to assess male fertility.
In practice, many men with normal sperm counts still experience infertility. The reason is simple: sperm must not only be present in adequate numbers but must also function properly.
Factors That Can Reduce Sperm Count
Based on data from WHO, ASRM, and the European Society of Human Reproduction and Embryology (ESHRE), reduced sperm count may result from various factors, including:
- Hormonal disorders (especially FSH and testosterone abnormalities)
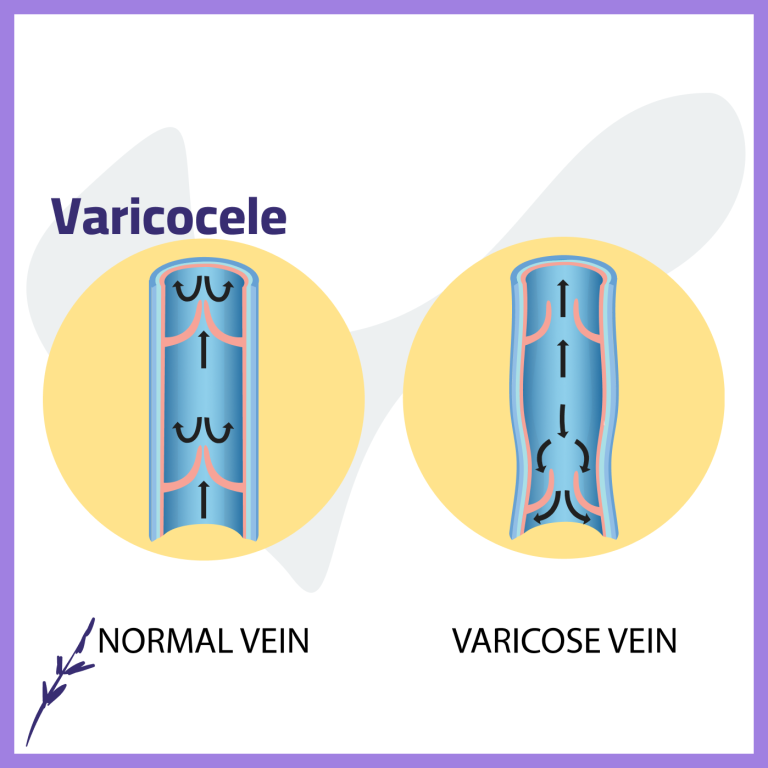
- Varicocele
- Genital tract infections
- Genetic conditions
- Smoking, alcohol, and drug use
- Overweight and obesity
- Chronic heat exposure
- Long-term stress and sleep disorders
- Certain medications and environmental toxins
The encouraging aspect is that many of these factors are modifiable or treatable, provided the underlying cause is correctly identified.
Why Focusing Only on the Number Can Be Misleading
From a clinical perspective, misinterpreting sperm count often leads to one of two outcomes:
- False reassurance in men with normal values
- Unnecessary anxiety in cases of mild reduction
Professional guidelines stress that treatment decisions should be based on a comprehensive evaluation, not a single isolated parameter.
Summary
Based on the most reliable international references:
- Sperm count is an important indicator of male reproductive health
- It is not sufficient on its own to diagnose fertility or infertility
- Accurate interpretation requires a holistic approach, considering multiple semen parameters and individual clinical context
👉 The number is the beginning of the journey—not the conclusion.