The effect of BMI on fertility
Body Mass Index (BMI) is one of the most important indicators of overall health, and its role becomes even more critical when it comes to reproductive health, fertility, and pregnancy outcomes. BMI reflects the relationship between a person’s height and weight and is widely used to assess whether an individual is underweight, within a healthy weight range, overweight, or obese. Although BMI does not directly measure body fat or metabolic health, it remains a practical and clinically useful tool in reproductive medicine.
Both high and low BMI can negatively affect fertility, increase pregnancy-related risks, and influence the health of the fetus and newborn. For this reason, evaluating and optimizing BMI before conception is strongly recommended for women who are planning a pregnancy.
How BMI Affects Fertility
High BMI and Fertility Challenges
A high BMI, particularly in the overweight and obese range, is associated with several mechanisms that can reduce fertility:
- Hormonal imbalance: Excess body fat alters estrogen, insulin, and leptin levels, which can disrupt ovulation and menstrual regularity.
- Insulin resistance: Common in overweight and obese individuals, insulin resistance can impair ovulation and is closely linked to conditions such as polycystic ovary syndrome (PCOS).
- Reduced egg quality: Metabolic and inflammatory changes associated with obesity may negatively affect egg development.
- Lower success rates with fertility treatments: Women with high BMI often experience reduced success rates with assisted reproductive technologies (ART) such as IVF.
In addition to fertility issues, obesity increases the time it takes to conceive and raises the likelihood of infertility even in women with regular cycles.
Low BMI and Fertility Risks
On the other end of the spectrum, a low BMI can also interfere with reproductive health:
- Energy deficiency: The body may suppress reproductive hormones when energy availability is too low.
- Irregular or absent ovulation: Underweight women are more likely to experience missed periods or anovulation.
- Reduced estrogen levels: Low estrogen can impair endometrial development and implantation.
Women with a very low BMI may struggle to conceive naturally and may face challenges maintaining a healthy pregnancy.
BMI and Pregnancy Outcomes
BMI not only influences the ability to conceive but also plays a major role in pregnancy safety and fetal development.
Risks Associated With High BMI During Pregnancy
Women who enter pregnancy with a BMI in the overweight or obese range have an increased risk of:
- Gestational diabetes
- High blood pressure and preeclampsia
- Cesarean delivery
- Pregnancy loss
- Large-for-gestational-age babies
- Birth complications and neonatal intensive care admission
Excess maternal weight can also affect the long-term metabolic health of the child, increasing the risk of obesity and metabolic disorders later in life.
Risks Associated With Low BMI During Pregnancy
Women who are underweight before pregnancy may face increased risks of:
- Low birth weight
- Preterm delivery
- Poor fetal growth
- Nutrient deficiencies
Adequate maternal weight and nutrition are essential to support placental function and fetal development throughout pregnancy.
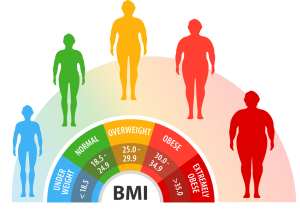
Understanding BMI Categories
BMI is calculated using the formula:
BMI = weight (kg) ÷ height² (m²)
Based on international guidelines, BMI categories are defined as:
- Underweight: BMI less than 18.5
- Normal weight: BMI between 18.5 and 24.9
- Overweight: BMI between 25 and 29.9
- Obesity: BMI 30 or higher
These categories are widely used to guide fertility counseling and pregnancy care.
Recommended Weight Gain During Pregnancy Based on BMI
Healthy weight gain during pregnancy is essential and depends on a woman’s pre-pregnancy BMI. These recommendations aim to balance fetal growth with maternal health and reduce pregnancy complications.
Underweight (BMI less than 18.5)
Women who are underweight before pregnancy are advised to gain 12.5 to 18 kilograms during pregnancy. This higher weight gain supports fetal growth and reduces the risk of low birth weight.
Normal Weight (BMI 18.5–24.9)
Women in the normal BMI range should aim to gain 11.5 to 16 kilograms. This range is associated with the lowest risk of pregnancy complications and optimal fetal outcomes.
Overweight (BMI 25–29.9)
Women who are overweight are generally advised to gain 7 to 11.5 kilograms. Controlled weight gain helps reduce the risk of gestational diabetes and high blood pressure while still supporting fetal development.
Obesity (BMI 30 or higher)
Women with obesity should limit pregnancy weight gain to 5 to 9 kilograms. Excessive weight gain in this group significantly increases pregnancy and delivery risks.
Why BMI Should Be Assessed Before Pregnancy
Checking BMI before conception allows women to make necessary lifestyle adjustments in advance, when changes are safer and more effective than during pregnancy. Improving BMI before pregnancy can:
- Increase the chance of natural conception
- Improve response to fertility treatments
- Reduce pregnancy complications
- Support healthier fetal growth
- Improve long-term health for both mother and child
Even modest weight changes—such as losing 5–10% of body weight in overweight women or gaining weight in underweight women—can significantly improve fertility and pregnancy outcomes.
Improving BMI Through Lifestyle Changes
Achieving a healthy BMI does not require extreme measures. Sustainable lifestyle changes are the most effective approach:
- Balanced nutrition: Focus on whole foods, adequate protein, healthy fats, and complex carbohydrates.
- Moderate physical activity: Regular, moderate exercise supports weight balance and hormonal health.
- Stress management: Chronic stress can interfere with weight regulation and reproductive hormones.
- Medical guidance: Healthcare providers can offer personalized advice, especially for women with metabolic or hormonal conditions.
BMI and Assisted Reproductive Technologies (ART)
BMI also affects outcomes in fertility treatments such as IVF and IUI. Abnormal BMI is associated with:
- Lower ovarian response
- Reduced egg and embryo quality
- Lower implantation and pregnancy rates
- Higher miscarriage risk
Optimizing BMI before starting ART can significantly improve success rates and reduce treatment-related risks.
Final Thoughts
Body Mass Index is a powerful yet modifiable factor that influences fertility, pregnancy safety, and fetal health. Both high and low BMI can disrupt reproductive function, increase pregnancy complications, and affect newborn outcomes.
For women planning pregnancy, assessing BMI and making appropriate lifestyle changes before conception is one of the most effective steps toward a healthy pregnancy and a healthy baby. By achieving and maintaining a BMI within the recommended range, women can support their reproductive health, improve fertility, and create the best possible environment for pregnancy and childbirth.