Age in failure of conception
Age is one of the most influential factors affecting fertility in both women and men. Although fertility does not suddenly disappear at a specific birthday, it gradually declines over time as a natural part of human biology. This decline becomes more noticeable after the mid-30s, particularly for women, but it also affects men in more subtle ways. Understanding how age influences fertility can help individuals and couples make informed decisions about family planning and reproductive health.
Fertility is shaped by a combination of biological, hormonal, genetic, and lifestyle factors. While age plays a central role, it does not act alone. Overall health, nutrition, stress levels, medical conditions, and genetic background all interact with age to determine an individual’s reproductive potential.
Why Fertility Declines With Age
Egg Quantity and Quality in Women
Women are born with a finite number of eggs, and no new eggs are produced after birth. Over time, both the number and quality of eggs decline. Each menstrual cycle involves the loss of multiple eggs, even though typically only one is ovulated. As age increases, the remaining eggs are more likely to have chromosomal abnormalities, which can reduce the chances of fertilization and increase the risk of miscarriage or genetic conditions.
By the mid-30s, the decline in egg quality accelerates. By the early 40s, the chances of producing a genetically healthy egg drop significantly, making natural conception increasingly difficult.
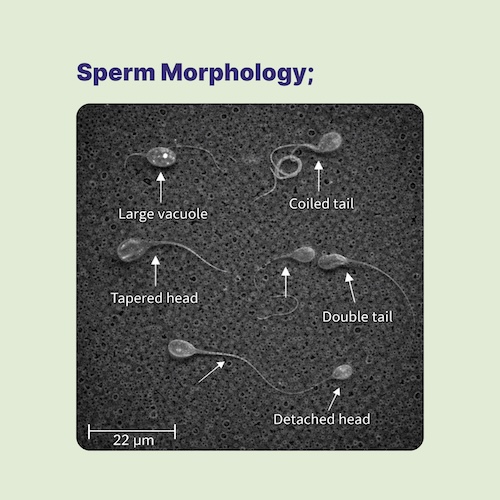
Sperm Changes in Men
Unlike women, men continue to produce sperm throughout their lives. However, male fertility is not immune to aging. With increasing age, sperm may show:
- Reduced motility (movement)
- Increased DNA fragmentation
- Higher rates of genetic mutations
- Decreased testosterone levels
Advanced paternal age has been associated with lower pregnancy rates, longer time to conception, and an increased risk of certain genetic and developmental conditions in offspring.
Natural Conception Rates by Age
Studies estimating average monthly chances of natural conception show a gradual decline with age. While these figures are averages and do not predict individual outcomes, they provide a general framework:
- Early to mid-20s: approximately 25–30% chance of pregnancy per cycle
- Late 20s to early 30s: approximately 15–20% per cycle
- Late 30s: around 10% per cycle
- Early 40s: about 5% per cycle
- Mid-40s and beyond: typically less than 1% per cycle
These statistics assume regular ovulation and no underlying fertility issues. Importantly, they do not account for male partner age, which can further influence outcomes.
Individual Variation in Fertility
Although age-related trends are well established, fertility is highly individual. Some people maintain good reproductive potential later into life, while others experience fertility challenges at a younger age. Factors contributing to this variation include:
- Genetic differences
- Ovarian reserve or sperm quality
- Past pregnancies or reproductive history
- Chronic health conditions
- Lifestyle factors such as smoking, alcohol use, diet, and stress
For this reason, age alone should not be used as the sole predictor of fertility potential.
Age and Pregnancy Risks
In addition to making conception more difficult, advancing age increases certain pregnancy-related risks, including:
- Higher rates of miscarriage
- Increased likelihood of chromosomal abnormalities
- Greater risk of pregnancy complications such as gestational diabetes and high blood pressure
These risks do not mean that healthy pregnancies are impossible at older ages, but they do highlight the importance of appropriate medical care and monitoring.
When to Seek Fertility Evaluation
General recommendations suggest:
- Individuals under 35 seek evaluation after 12 months of trying to conceive
- Individuals over 35 seek evaluation after 6 months
- Individuals over 40 consider early consultation, even before attempting conception
A fertility specialist can assess ovarian reserve, sperm quality, hormonal balance, and overall reproductive health to provide personalized guidance.
Options for Addressing Age-Related Infertility
Modern reproductive medicine offers a range of options to help individuals and couples overcome age-related fertility challenges.
Ovulation Induction
Medications may be used to stimulate the ovaries and improve the timing and consistency of ovulation.
Intrauterine Insemination (IUI)
IUI involves placing prepared sperm directly into the uterus around the time of ovulation, increasing the chance of fertilization.
In Vitro Fertilization (IVF)
IVF bypasses several natural barriers by fertilizing eggs in a laboratory and transferring embryos into the uterus. IVF success rates decline with age but remain one of the most effective options for many people.
Intracytoplasmic Sperm Injection (ICSI)
ICSI is a specialized form of IVF in which a single sperm is injected directly into an egg, often used when sperm quality is reduced.
Preimplantation Genetic Testing (PGT)
PGT allows embryos to be screened for chromosomal abnormalities before transfer, reducing miscarriage risk and increasing the chance of a healthy pregnancy, especially at older ages.
Egg Donation
Using eggs from a younger donor can significantly improve pregnancy success rates for women with age-related decline in egg quality.
Sperm Donation
Sperm from a younger donor may be an option when male age or sperm quality is a limiting factor.
Embryo Donation
Embryos created by other individuals or couples can be transferred to the uterus as an alternative path to pregnancy.
Adoption
For some, adoption provides a fulfilling path to parenthood that does not involve biological reproduction.
Planning Ahead and Fertility Preservation
For individuals who wish to delay childbearing, fertility preservation, such as egg or sperm freezing, may help protect reproductive options for the future. Freezing eggs or sperm at a younger age preserves genetic material before age-related decline occurs.
Final Thoughts
Age is a powerful but not absolute determinant of fertility. While fertility naturally declines over time, individual outcomes vary widely, and modern medicine offers many options to support family-building at different stages of life. Early education, proactive planning, and timely medical guidance can make a meaningful difference.
If you are thinking about starting a family—now or in the future—seeking accurate information and professional advice can help you navigate age-related fertility changes with confidence and clarity.